- Visibility 703 Views
- Downloads 273 Downloads
- Permissions
- DOI 10.18231/j.jco.2024.079
-
CrossMark
- Citation
Evaluation of probiotic, chlorhexidine, and fluoride mouthwashes in orthodontic preventive care- A unicentric three-arm parallel randomized controlled trial
Abstract
Introduction: Fixed orthodontic appliance therapy can lead to increased plaque accumulation, gingivitis, and white spot lesions (WSL) due to difficulties in maintaining proper oral hygiene.
Objective: This study aims to compare the effectiveness of three different mouthwashes—Probiotic, Fluoridated, and Chlorhexidine (CHX) mouthwashes, in reducing plaque formation, gingivitis, and WSL during the early stages of orthodontic treatment.
Materials and Methods: A randomized, three-arm-parallel study was conducted with 72 subjects undergoing fixed orthodontic therapy, divided equally into three active groups without a control group. Group I used Probiotic mouthwash, Group II used 0.2% Sodium fluoride mouthwash, and Group III used 0.2% Chlorhexidine mouthwash. Gingival Index (GI), Orthodontic Plaque Index (OPI), Bleeding on Probing (BOP), and WSL were assessed at baseline just before bonding procedures (T0), 4 weeks (T1), 8 weeks (T2), and 12 weeks (T3). Interventions were administered from T1 to T2 for 4 weeks and withdrawn. Intergroup and intra-group comparisons across the groups were assessed by non-parametric Kruskal-Wallis and Friedman tests.
Results: Intra-group improvements in OPI, GI, BOP, and WSL over time for all three groups during the given study period. Probiotic mouthwash showed the most substantial reduction in BOP (34% from baseline), followed by chlorhexidine (19%), and fluoride (11%) at the end of the 12th week. Fluoride mouthwash was most effective in reducing the OPI (15% from baseline) and WSL(4%), while chlorhexidine was most effective in reducing the GI (15% from baseline). Inter-group comparisons revealed no statistically significant differences in the effectiveness of the three mouthwashes.
Conclusion: All three mouthwashes improved oral hygiene indices over time, there were no significant differences between the probiotic, fluoridated, and chlorhexidine groups in their overall effectiveness.
Introduction
Fixed orthodontic appliance therapy is a widely used treatment aimed at correcting dental abnormalities by aligning teeth in all three dimensions. The presence of attachments on the tooth surface invites plaque formation and makes self-cleansing difficult.[1] This increase in retention areas for plaque around bands and brackets leads to changes in the oral environment, causing reactions in the gingiva and periodontal breakdown.[1], [2] The placement of fixed orthodontic appliances severely impedes tooth brushing, makes conventional oral hygiene more difficult, and creates areas for bacterial adhesion and biofilm formation. [3] Additionally, plaque and calculus, primarily consisting of salivary mineral particles and bacteria such as Lactobacillus and Streptococcus mutans, can further complicate dental health by demineralizing enamel and causing white spot lesions (WSL). [2], [3], [4] The prevalence of WSL was noted to be 2-96% among the patients undergoing orthodontic treatment depending on the detection method. They started appearing within four weeks and were more prevalent in the first six months of the start of orthodontic treatment. [5], [6] The WSL was noted irrespective of whether self-ligating or conventional brackets were used. [7] Control of dental microbial biofilm causing gingivitis can be achieved by various chemical and mechanical methods that interrupt, reduce, or eliminate the microorganisms. Among these, the mechanical removal of microbial biofilm using toothbrushes with dentifrices is the most common way of controlling gingivitis. Despite this, patients often have difficulty maintaining an acceptable level of oral hygiene, which cannot be achieved by mechanical methods alone. [8] Due to the inefficiency of mechanical methods in maintaining proper oral hygiene, chemical methods, such as mouthwash solutions containing antimicrobial agents, have evolved to ensure effective oral hygiene maintenance. [2] The use of chemical agents as an adjunctive to brushing proved much more effective in controlling gingivitis in a better way, as brushing helps in reducing the biofilm while it cannot act on microflora affecting the gingival tissue which can be overcome by chemical agents. [9]
Chlorhexidine(CHX) is a gold-standard chemotherapeutic agent known for its antibacterial, antiplaque, and antigingivitic properties. [10] When used as a mouthwash or topical oral gel, chlorhexidine (CHX) can cause unpleasant effects such as dry mouth (xerostomia), altered taste sensations (hypogeusia), desquamation of the oral mucosa, staining, and smoothing of composite materials. However, the main undesirable consequence that dissuades patients from using CHX mouthwash is likely teeth staining. [11] These drawbacks have spurred the development of more natural and biocompatible agents, such as fluorides and probiotics, which help maintain oral health and prevent new caries when oral hygiene is challenging.
Topical fluoride is well known for its impact on limiting demineralization and increasing remineralization of tooth hard tissue, particularly in early carious lesions. [12] Low fluoride concentrations, such as those in fluoride toothpaste, produce optimal results and are associated with a significant reduction in caries. An earlier study established that a daily rinse of fluoride mouthwash is effective in reducing white spot lesions during the initial first three months of orthodontic treatment. [13]
Probiotics, live microorganisms that balance our microbiomes and boost immunity, are gaining recognition recently for their role in oral health. [14], [15] They can reduce dental caries by suppressing oral pathogens and modulating the microbial makeup of dental plaque. Probiotics work through various mechanisms, including antagonistic activity against pathogens, coaggregation, growth inhibition, and production of bacteriocins, organic acids, and hydrogen peroxide. This results in reduced pathogenicity and cariogenic potential of biofilm microorganisms. Strains like Lactobacillus casei, Lactobacillus rhamnosus, Lactobacillus reuteri, and Bifidobacterium species are effective in blocking cariogenic bacteria and their colonization, thus preventing dental caries and gingivitis. [14]
A review of the literature reveals that only one such study has been documented on the effectiveness of probiotic mouthwashes in orthodontic patients in comparison to chlorhexidine mouthwash. [15] The current study was taken to compare the gingival health parameters in three different groups of orthodontic patients who were prescribed three different three mouth rinses containing probiotics, fluoridated mouthwash, and chlorhexidine. This study was also designed to evaluate the effectiveness during the withdrawal period. The null hypothesis of this study is that there is no difference in the remineralizing and plaque-inhibiting properties of these three mouthwashes during the initial stages of fixed orthodontic treatment.
Material and methods
This three-arm parallel randomized controlled trial was carried out in the Department of Orthodontics, Narayana Dental College, India from October 2022 to September 2023. The ethical committee reviewed and approved the study (IECNDCH/2022/Mar/P-28), and the trial was registered with the National Trial Registry (REF/2023/11/075868).
The sample of this study was drawn from cohort groups who were due for the start-up of fixed appliance orthodontic treatment. The sample size calculation was done using G Power version 3.1.9.6. A minimum of 42 subjects divided into three equal treatment groups provides 80% power with a 5% error and a 95% confidence interval (CI). The study included a final sample of 72 subjects equally divided into three groups of 24 each (Figure 1).

Healthy patients aged 18-30 with good oral hygiene complete permanent dentition (up to first molars) and minimal crowding were selected. Patients with a history of smoking, systemic diseases, medication allergies to accessories, and poor oral hygiene were excluded. Those meeting the inclusion criteria were informed about the procedure and encouraged to participate. Informed permission and assent were obtained from consenting subjects.
All patients were bonded with the MBT bracket system (3MTM Victory Series TM). Before the study, all cavities were restored, and gingival conditions were normalized. Randomization and allocation were conducted using the Fish-bowl method. [16] This process was carried out by a nursing staff member. The allocator was unaware of the study's objectives. Subsequently, the primary investigator/assessor, who remained blinded to the allocation, measured the outcomes post-intervention. The study was primarily single-blinded but effectively double-blinded as both participants and the assessor of scores were unaware of group assignments. Patients were equally assigned to all three groups, with n=24 in each group (Figure 2).
1. Group I: Probiotic mouthwash (perfora® mouthwash with Bacillus coagulans bacterium, Chipper Consumer Pvt. Ltd. India).
2. Group II: 0.2% Fluoridated mouthwash (Colgate®- PreviDent rinse, 0.2% sodium fluoride mouthwash, Colgate-Palmolive, India).
3. Group III: 0.2% Chlorhexidine mouthwash (Aloorigold®, 0.2 %Chlorhexidine gluconate Bhavani pharmachem pvt ltd India).

The study duration was extended for a total of 12 weeks – T0 (just before bonding procedures); T1- 4 weeks; T2- 8 weeks; T3-12 weeks. The brushing instructions were given after bonding procedures. After brushing their teeth, patients were advised to vigorously rinse with only plain water during the first four weeks ( T0-T1). Only non-fluoridated toothpastes were recommended during this period. The intervention begins after the first appointment, typically after 28 days or the initial follow-up visit at T1. Patients were instructed by the orthodontist on how to rinse the given mouthwash. After brushing their teeth, patients were advised to vigorously swish their mouth with 10ml of the solution for 30 seconds and then spit it out. They were instructed not to eat or drink for 30 minutes after rinsing. The patients were daily reminded of the regimen by an automated message system once on the previous night and early morning of the same day on using the mouth rinses through a mobile app. After one month of usage, at the end of the 8th week (T2), patients were instructed to withhold the use of the mouth rinsing from T2 to T3.
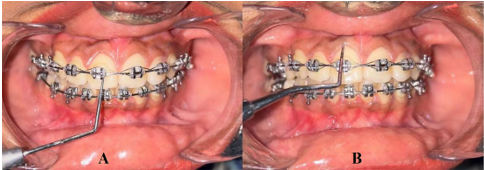
The Gingival parameters and WSL were recorded at T0, T1, T2, and T3. The primary outcome assessment, gingival health and bleeding on probing (BOP) was done with Sillness and Loe Gingival Index (GI). [17] Secondary outcome of plaque formation was measured with the Orthodontic Plaque Index (OPI). [18] The WSL index of Gorelick [19] assessed the demineralization areas. The WSL, BOP, OPI, and GI are calculated as ordinal data by examining the four surfaces of each tooth (mesiofacial, facial, distofacial, lingual), and averaged to derive the mean values of the teeth examined. If bleeding occurs within ten seconds, it is recorded as positive, if not, recorded as negative. Negative scoring is equivalent to the gingival index score of 0 and 1. A positive recording is equivalent to the gingival index score of 2 and 3. Bleeding on the probing index is measured in percentage, calculated by the total teeth that bleed during probing by total teeth examined (Figure 3).
Examiner calibration: Initial training was provided to the primary investigator (SR) to assess the WSL scores and OPI by an experienced person (MP) who had formal training in International Caries Detection and Assessment System (ICDAS) assessment and was involved in similar research activities. Calibration of the primary investigator was performed with the trainer and Kendall's coefficient of concordance (Kendall's W) values above 0.92 for interexaminer and intraexaminer reproducibility were achieved.
All the patients completed the study period without any adverse reactions and completed the treatments with prescribed mouthwashes. The patients were advised to use the fluoridated toothpaste after the study period.
Statistical Analysis
All the collected data was inputted into a Microsoft Excel spreadsheet (MS Office 2018). The normality of data was assessed by the Kolmogorov-Smirnov test (KS) and non-parametric tests analyzed the data. The Statistical data was analyzed by online statistics software (DATAtab, Graz, Austria). Friedman’s test compared within-group differences between the indices at different periods. Kruskal Wallis test was used for inter-group comparison followed by the post-hoc Bonferroni test for pairwise comparisons. Bleeding on probing (BOP) was analyzed as bi-nominal data and inter and intra-group comparisons were done using Cochran’s Q test. A significance level of p < 0.05 was chosen for all statistical tests.
|
|
Group-I Probiotic (n=24) |
Group-II Fluoride (n=24) |
Group-III chlorhexidine (n=24) |
Test statistic |
|
Age in years |
ANOVA |
|||
|
Mean |
20.95 |
21.25 |
20.87 |
F=0.081 p=0.92 |
|
SD |
2.99 |
4.32 |
2.57 |
|
|
|
||||
|
Gender wise distribution |
Chi-square test |
|||
|
Male |
8 |
4 |
6 |
χ2=2.71 Df=2 p=0.25 |
|
Female |
16 |
20 |
18 |
SD-standard deviation; *p≤0.05 statistically significant. Age distribution is calculated using ANOVA. Gender distribution is calculated using the Chi-Square test df- degree of freedom
|
Group (n-=24) |
|
Gingival Index (GI) |
Orthodontic Plaque Index ( OPI) |
White spot lesion ( WSL) |
Bleeding on probing (BOP) |
||||
|
Mean |
SD |
Mean |
SD |
Mean |
SD |
Mean |
SD |
||
|
Group-I Probiotic (n=24) |
T0 |
0.25 |
0.53 |
0.02 |
0.06 |
0 |
0 |
0.13 |
0.34 |
|
T1 |
0.21 |
0.51 |
0.53 |
0.37 |
0 |
0 |
0.29 |
0.46 |
|
|
T2 |
0.25 |
0.68 |
0.46 |
0.47 |
0.04 |
0.2 |
0.13 |
0.34 |
|
|
T3 |
0.17 |
0.48 |
0.43 |
0.36 |
0 |
0 |
0.08 |
0.28 |
|
|
Group-II Fluoride (n=24) |
T0 |
0.17 |
0.48 |
0 |
0 |
0.04 |
0.2 |
0.21 |
0.41 |
|
T1 |
0.25 |
0.53 |
0.45 |
0.24 |
0.04 |
0.2 |
0.21 |
0.41 |
|
|
T2 |
0.21 |
0.51 |
0.45 |
0.28 |
0 |
0 |
0.13 |
0.34 |
|
|
T3 |
0.17 |
0.48 |
0.27 |
0.12 |
0 |
0 |
0.13 |
0.34 |
|
|
Group-III chlorhexidine (n=24) |
T0 |
0.29 |
0.46 |
0 |
0 |
0 |
0 |
0.25 |
0.44 |
|
T1 |
0.33 |
0.56 |
0.47 |
0.35 |
0 |
0 |
0.29 |
0.46 |
|
|
T2 |
0.25 |
0.68 |
0.38 |
0.3 |
0 |
0 |
0.17 |
0.38 |
|
|
T3 |
0.25 |
0.53 |
0.02 |
0.06 |
0 |
0 |
0.13 |
0.34 |
|
Group- (n=24)
|
Parameter |
Mean ranks |
χ2 |
df |
p-value |
|
||
|
T0 |
T1 |
T2 |
T3 |
|||||
|
Group-I Probiotic (n=24) |
GI |
2.58 |
2.48 |
2.54 |
2.4 |
0.28 |
3 |
0.9 |
|
OPI |
1.02 |
3.42 |
2.75 |
2.81 |
45.91 |
3 |
0.01* |
|
|
WSL |
2.48 |
2.56 |
2.48 |
2.48 |
0.08 |
3 |
0.9 |
|
|
BOP |
2.44 |
2.77 |
2.44 |
2.35 |
1.48 |
3 |
0.68 |
|
|
Group-II Fluoride (n=24) |
GI |
2.44 |
2.6 |
2.52 |
2.44 |
0.28 |
3 |
0.96 |
|
OPI |
1 |
3.52 |
3.13 |
2.35 |
55.34 |
3 |
0.01* |
|
|
WSL |
2.54 |
2.54 |
2.46 |
2.46 |
0.1 |
3.0 |
0.99 |
|
|
BOP |
2.58 |
2.58 |
2.42 |
2.42 |
0.4 |
3 |
0.94 |
|
|
Group-III chlorhexidine (n=24) |
GI |
2.63 |
2.67 |
2.42 |
2.29 |
1.35 |
3.0 |
0.71 |
|
OPI |
1 |
3.33 |
2.85 |
2.81 |
45.61 |
3 |
0.01* |
|
|
WSL |
2.5 |
2.5 |
2.5 |
2.5 |
0.0 |
3.0 |
1.0 |
|
|
BOP |
2.58 |
2.67 |
2.42 |
2.33 |
1.0 |
3.0 |
0.80 |
|
Group |
Intra-pair comparison between different periods |
Rank sums difference |
Standard error |
Adj. p |
|
|
Group-I Probiotic (n=24) |
T0 |
T1 |
-2.4 |
0.37 |
<.001* |
|
T0 |
T2 |
-1.73 |
0.37 |
<.001* |
|
|
T0 |
T3 |
-1.79 |
0.37 |
<.001* |
|
|
Group-II Fluoride (n=24) |
T0 |
T1 |
-2.52 |
0.37 |
<.001* |
|
T0 |
T2 |
-2.12 |
0.37 |
<.001* |
|
|
T0 |
T3 |
-1.35 |
0.37 |
.001* |
|
|
Group-III chlorhexidine (n=24) |
T0 |
T1 |
-2.33 |
0.37 |
<.001* |
|
T0 |
T2 |
-1.85 |
0.37 |
<.001* |
|
|
T0 |
T3 |
-1.81 |
0.37 |
<.001* |
|
Parameter |
Time |
G-I -P |
G-II F |
G-III CHX |
H- statistic χ2 |
df |
p-value |
|
Gingival Index (GI) |
T0 |
36.6 |
33.69 |
39.21 |
1.68 |
2.0 |
0.43 |
|
T1 |
34.58 |
36.02 |
38.9 |
1.01 |
2.0 |
0.64 |
|
|
T2 |
36.52 |
36.46 |
36.52 |
0 |
2.0 |
1.0 |
|
|
T3 |
36.5 |
36.5 |
36.5 |
0 |
2 |
1 |
|
|
Orthodontic Plaque Index (OPI) |
T0 |
38.5 |
35.5 |
35.5 |
4.06 |
2 |
0.132 |
|
T1 |
38.83 |
36 |
34.67 |
0.5 |
2 |
0.77 |
|
|
T2 |
35.38 |
39.98 |
34.15 |
1.04 |
2 |
0.59 |
|
|
T3 |
41.79 |
27.69 |
40.02 |
6.54 |
2 |
0.38 |
|
|
White Spot Lesion(WSL) Index |
T0 |
36 |
37.5 |
36 |
2 |
2 |
0.36 |
|
T1 |
37 |
37 |
35.5 |
1.01 |
2.0 |
0.60 |
|
|
T2 |
36.5 |
36.5 |
36.5 |
NaN |
NaN |
NaN |
|
|
T3 |
36.5 |
36.5 |
36.5 |
NaN |
NaN |
NaN |
|
|
Bleeding on probing (BOP) |
T0 |
34 |
37 |
38.5 |
1.22 |
2 |
0.542 |
|
T1 |
37.5 |
34.5 |
37.5 |
0.56 |
2 |
0.75 |
|
|
T2 |
36 |
36 |
37.5 |
0.23 |
2 |
0.89 |
|
|
T3 |
35.5 |
37 |
37 |
0.28 |
2 |
0.87 |
|
Groups (n=24) each |
Condition present/ Absent |
TIME |
|
||||
|
Group -I (P) (Probiotic) |
T0 |
T1 |
T2 |
T3 |
Total |
Intra group comparison |
|
|
Present |
21 |
17 |
21 |
22 |
81 |
Chi2 -4.66 df 3 p -0.19 |
|
|
Absent |
3 |
7 |
3 |
2 |
15 |
||
|
Group -II (F) (Fluoride) |
Present |
19 |
19 |
21 |
21 |
80 |
Chi2 -1.2 df 3 p -0.19 |
|
Absent |
5 |
5 |
3 |
3 |
16 |
||
|
Group -III(CHX) (Chlorhexidine) |
Present |
19 |
19 |
19 |
19 |
76 |
Chi2- 1.2 df 3 p 0.75 |
|
Absent |
5 |
5 |
5 |
5 |
20 |
||
|
Column total per group |
24 |
24 |
24 |
24 |
96 |
|
|
|
Intergroup comparison |
P-Value |
p – 0.55 |
-0.75 |
p 0.84 |
p -0.86 |
|
Results
The present study included 72 participants (n=24 per group; male: 18, female: 54). There was no variation between the groups regarding gender (p=0.92), and age distribution (p=0.25)
([Table 1]). Descriptive data for GI. OPI, Bleeding on Probing (BOP), and White Spot Lesions (WSL) were collected at multiple time points ([Table 2]).
All the indices increased from T0 to T1 in all the groups except a non-significant decrease for probiotic mouthwash. Within-group comparisons between the different periods demonstrated no statistical differences between the different durations except for OPI, which is significant in all groups (p < 0.05) ([Table 3]). Post hoc Bonferroni tests revealed significant differences (p < 0.001) at T0-T1, T0-T2, and T0-T3 within each group for OPI ([Table 4]).
Inter-group comparisons for each time point employed Kruskal-Wallis tests, showing no significant differences at individual time points for all indices ([Table 5]).For meaningful analytical purposes, the BOP was converted into binomial data and expressed as percentages for the presence and absence of bleeding on probing ([Table 6]). Cochran’s Q test for intra and inter-group BOP comparisons found no significant differences between the groups at a given interval as well as across the four-time points within each group ([Table 6]).
Discussion
Fixed orthodontic treatment corrects various types of malocclusion and skeletal deformities by using components bonded or banded to tooth surfaces to move teeth into desired positions. These components include archwires made from different materials (such as stainless steel, and nickel-titanium) and elastics on bonded metal brackets. The attachments on tooth surfaces during fixed orthodontic therapy make it challenging for individuals to maintain proper oral hygiene through mechanical methods like brushing, facilitating the accumulation of oral microbial flora and leading to gingival inflammation. This study evaluated the efficacy of new biological probiotic mouthwash with that of existing chlorhexidine and fluoride mouthwashes performed across different time frames during the initial stage of fixed orthodontic therapy. Various indices were used to assess the gingival inflammation and initiation of demineralized lesions during this study period. The study included an intervention period as well as a withdrawal period to assess the substantiated action of the mouthwashes.
We implemented an observation interdiction period, denoted as T0-T1, for all the groups. This period occurred after standardizing the brushing procedures for all the individuals. No intervention was provided during this period. The purpose of this study is to investigate whether orthodontic appliances inherently promote the build-up of plaque. Furthermore, each group has served as a self-control group in our study throughout this period. In all the groups we noticed a deterioration of gingival health parameters at T1 compared to T0. We found no significant differences in indices between groups at T1, where the intervention started (Table 3).
We have only one previous study to compare our results with, which examined the use of probiotic mouthwashes on patients undergoing orthodontic treatment. [15] The investigators assessed the impact of probiotic and chlorhexidine mouthwashes on the levels of streptococcus mutans. They observed a reduction of S mutans levels over a 4 week period of daily use of probiotic mouth rinse. The researchers used probiotic mouthwashes made by mixing sporlac sachets with distilled water. The mouthwashes contained 2 × 10 [8] colony-forming units (CFU)/g of Lactobacillus sporogenes. They assessed the gingival and plaque parameters. The probiotic utilized in our investigation is specifically prepared with Bacillus coagulans at a concentration of 3.3 X 10 [6] CFU/ml. While it is not possible to directly compare the two studies, we attempted to establish a connection between them. In addition, we have conducted a comparative analysis of our findings with prior research that assessed the gingival health of orthodontic patients who were given chlorhexidine and fluoride mouthwashes.
I.Gingival Index (GI) ([Table 2], [Table 3]): In the probiotic group, the mean GI value decreased from 0.25 at baseline to 0.17 at the end of our study. Overall a reduction of 16% in the gingival inflammation in noted after the end of the study. However, an increase in the index values between T1- T2 values increased in this group. This indicates the probiotic action may be slow in action compared to the other groups where such change is not noticed for the given period.
In the fluoride group, we noticed a decrease in the gingival index immediately after intervention with T1 (0.25 ± 0.53) and T2 (0.21 ± 0.51). Further, a decrease in the GI was noticed during the withholding period suggesting improved gingival health over time with T3 (0.17 ± 0.48). A previous study [13] reported a decrease of 0.3 In the GI scores after three months of 0. 2% of Sodium Fluoride (NaF) in orthodontic patients.
For the chlorhexidine group, a reduction of 32 % in the gingival inflammation is noted immediately after the intervention period at T2 compared to T1 (0.33), but no carry-over action is noticed between the T2 and T3(0.25, 0.25) when the mouth rinse is withdrawn. The findings of the present study are consistent with earlier studies of chlorhexidine mouthwash in orthodontic patients. The studies reported a decrease in the GI ranging from 0.17 to 0.54 immediately after 3-4 weeks of intervention. [15], [20], [21] A previous study [21] reported the effect of chlorhexidine after a relapse period of 15 days. The findings are similar to our study substantiating the continued action of the chlorhexidine for 4 weeks after withholding mouth rinsing regimen.
Only one comparative study by Shah [15] evaluated the efficacy of probiotics and chlorhexidine in orthodontic patients. They reported a mean decrease in GI index higher in the probiotic group compared to the chlorhexidine after 3 weeks of intervention. In contrast, chlorhexidine reported more beneficial effects immediately after intervention compared to probiotic mouthwash. In fact, during this period the GI increased from 0.21(T1) to 0.25 (T2).
II. Orthodontic Plaque Index (OPI) ([Table 2], [Table 3], [Table 4]): In all the groups, the OPI index increased significantly immediately after fixed appliance therapy as measured from T0 to T1 by about 0.4. This may be attributed to the components of the appliance which acts as a source of plaque accumulation. This rise could be due to various factors, including inadequate oral hygiene, dietary habits, or the presence of fixed orthodontic appliances. In the probiotic mouthwash group, OPI values remained the same immediately after the intervention (T2- 0.46 ± 0.47) and the retraction period (T2.46 ± 0.36) indicating continued plaque formation despite of usage of the mouthwash. Despite the increase in plaque accumulation, we noticed a decreased GI index during this period but this is the only group that reported initiation of WSL during this given time interval compared to the other groups. This may be attributed to the microbiological nature of the plaque which needs further exploration by future studies. In contrast to our study, Shah [15] reported a mean reduction of the Plaque index from 0.78 at baseline to 0.18 after three weeks of a probiotic daily mouth rinse regimen.
The fluoride mouthwash group (Group II) showed no change in orthodontic plaque index during the intervention period but a substantial decrease at the end of the study (T3- 0.21 ± 0.45) compared to T1 (0.45 ± 0.24). The findings are similar to the previous study [22] but with different variables. The study compared Amide fluoride and Stannous fluoride toothpaste and mouth rinse, noting significant reductions in plaque build-up and improvement in gingival health (P < 0.05). For fluoride toothpaste alone, the plaque index decreased by 1.2, and for the combination with mouth rinse, it decreased from 2.21 ± 0.52 to 1.32 ± 0.42.
In the chlorhexidine mouth rinse group (Group III), the orthodontic plaque index scores after an initial increase at T1(0.47± 0.35) declined to T2 (0.38± 0.3) and finally 0.02± 0.06. The reduction in plaque may be considered due to the antimicrobial nature of chlorhexidine.
Studies by Raju[21] and Abrol[23] reported mean decreases in plaque index after using chlorhexidine mouth rinse as 0.20 and 0.10, respectively. In contrast, Malik[24] reported significantly higher reductions with decreases of 12.15 and 12.95, respectively. These variations could be due to differences in study design, concentration and formulation of chlorhexidine mouth rinse, participants' oral hygiene practices, baseline plaque levels, and demographic factors.
Shah[15] reported a significant and similar decrease in Plaque Index values for both probiotic and chlorhexidine groups compared to the control group. Specifically, the chlorhexidine group saw a reduction from 0.88 at baseline to 0.34 after three weeks of intervention. Similarly, the probiotic group's mean Plaque Index value dropped from 0.78 at baseline to 0.18. This finding is not in tune with the findings of the present study.
III. White Spot Lesion (WSL) ([Table 2], [Table 3]): No significant demineralization spots were noted for any of the three groups during the observation period indicating the anti-cariogenic nature of all three groups. In the probiotic group, there was an increase in the mean value from T0 to T1 (day 1 to week 4), rising from 0 ± 0 to 0.04 ± 0. This was followed by a decrease from T1 to T3 (week 4 to week 12). In a similar study[24] daily consumption of probiotic lozenges did not significantly affect the development of WSL during orthodontic treatment with fixed appliances. The fluoride mouthwash group exhibited an increase in the white spot lesion index from T0 to T1, with values constant at 0.04 ± 0. At subsequent time points T2 and T3, the index decreased to 0, suggesting the gradual remineralization of white spot lesions with continued fluoride use. Another study [25] found a significantly lower incidence of WSL in the fluoride group compared to the placebo group (P = 0.038). In contrast, yet another study found an increase in the rise of WSL despite fluoride mouth rinse in the initial first two months of start-up of orthodontic fixed appliances. [13] The study reported a decrease in the WSL indices after 2 months of the intervention probably due to remineralisation of the previous lesions. The study also reported that APF is more effective than neutral 0.2% sodium fluoride in preventing WSL and gingivitis during orthodontic treatment.
IV. Bleeding on probing (BOP) ([Table 2], [Table 3], [Table 6]): The frequency of bleeding increased in the immediate first month of wearing the fixed appliance. The increase in BOP indices may be correlated to the gingival inflammation resulting from accumulation of the plaque. After the intervention, scores decreased from T1 to T3 (12 weeks), indicating a reduction in BOP and suggesting the effectiveness of the probiotic mouthwash in improving gingival health. Comparative studies support these findings to varying extents. Another investigation [26] observed a statistically significant decrease in gingival bleeding using probiotic tablets in pediatric patients under 10 years after a three-month trial. Conversely, in a study, Seide [27] found that while probiotics improved clinical parameters in periodontal therapy, they had no positive effects on white spot lesions (WSL), gingival indices, or BOP during orthodontic treatment with fixed appliances. However, another study [28] reported that in orthodontic patients aged 18 to 30 years, salivary nitric oxide was a significant marker of gingival inflammation, and probiotics, alongside non-surgical periodontal therapy (NSPT), reduced gingival inflammation and plaque formation during orthodontic treatment.
The present research indicates that BOP index scores in the fluoride mouthwash group remained constant from T0 (0.21 ± 0.41) to T1 (4 weeks), but decreased from T1 to T3 (12 weeks), suggesting improved gingival health over time. In another study [29] they found that while gingival bleeding scores were significantly higher at 12, 18, and 24 months compared to baseline in orthodontic patients, this was not statistically significant for those using fluoride rinse.
The reduction BOP index with chlorhexidine observed in our study is in concordance with the previous study, [30] where CHX mouthwash (0.12%) was administered twice a week for 60 days to adult orthodontic patients, resulting in a significant reduction in plaque, gingival, and gingival bleeding indexes (P < 0.05) over various evaluation periods. Similarly, Brightman [31] found that using CHX mouthwash (0.12%) twice daily for four months in orthodontic patients significantly reduced plaque accumulation (MD = -0.44, p = 0.04), though it had no significant effect on gingival health or bleeding.
In the present study, Probiotic mouthwash showed the most substantial reduction in bleeding on probing (BOP), achieving a 34% decrease from baseline. Chlorhexidine (CHX) followed closely with a 19% reduction, while Fluoride exhibited the least effectiveness with an 11% reduction in BOP.
In summary, the probiotic mouthwash is as effective as chlorhexidine and fluoride rinses in improving gingival health in orthodontic patients, and hence the null hypothesis stands rejected. Overall, while each intervention improved specific oral health indices within their groups, there were no significant differences between the probiotic, fluoride, and chlorhexidine mouthwash groups in terms of overall oral plaque index or bleeding on probing.
However, no significant differences were noted between the groups for a given time interval (Table 5). Probiotic mouthwashes were slow in the onset of action. All three groups exhibited effectiveness in the withdrawal period to a similar extent. Comparatively, fluoride has long and sustained protective action. In general, chlorhexidine was most effective in the reduction of GI and against plaque formation.
Limitations
The study has inherent limitations due to its design with three active intervention arms and no additional control group for comparison, which could have raised ethical concerns in orthodontic patient care if involved. We have not measured the levels of cariogenic bacteria at various periods during the study. The study focused only on patients with low to moderate gingival inflammation risk, thus excluding those at high risk or with poor oral hygiene, limiting evaluation of potential mouth rinse protective effects. Despite regular patient checks and reminders for material usage, adherence may have been inconsistent. Extending the study duration and increasing the sample size would allow for more thorough, long-term evaluations and future studies should explore the efficacy of additional probiotics in orthodontic care. Future trials should identify oral regions requiring more hygiene focus, particularly in areas with higher crowding and plaque accumulation. Research on older adults undergoing orthodontic treatment is essential due to their elevated periodontal issues.
Conclusion
Fixed orthodontic appliances are inevitably associated with plaque accumulation. Probiotics mouthwash is as effective as chlorhexidine and fluoride rinses in improving gingival health during the initial stages of fixed orthodontic treatment.
Source of Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests
The author(s) declared no conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- O'reilly MM, Featherstone JD. Demineralization and remineralization around orthodontic appliances: an in vivo study. Am J Orthod Dentofacial Orthop. 1987;92(1):33-40. [Google Scholar]
- Lundström F, Krasse B. Caries incidence in orthodontic patients with high levels of Streptococcus mutans. Eur J Orthod. 1987;9(2):117-138. [Google Scholar]
- Sari E, Birinci I. Microbiological evaluation of 0.2% chlorhexidine gluconate mouthrinse in orthodontic patients. The Angle Orthod. 2007;77(5):881-5. [Google Scholar]
- Sakamaki S, Bahn A. Effect of orthodontic banding on localized oral lactobacilli. J Dent Res. 1968;47(2):27-84. [Google Scholar]
- Gorelick L, Geiger A, Gwinnett A. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982;81(2):93-101. [Google Scholar]
- Tufekci E, Dixon J, Gunsolley J, Lindauer S. Prevalence of white spot lesions during orthodontic treatment with fixed appliances. Angle Orthod. 2011;81(2):206-16. [Google Scholar]
- Mde A, Saraiva P, Maltagliati L, Rhoden F, Costa C, Normando D. Alterations in plaque accumulation and gingival inflammation promoted by treatment with self-ligating and conventional orthodontic brackets. Dental Press J Orthod. 2015;20(2):35-41. [Google Scholar]
- Rakhshan H, Rakhshan V. Effects of the initial stage of active fixed orthodontic treatment and sex on dental plaque accumulation: a preliminary prospective cohort study. Saudi J Dent Res. 2015;6(2):86-90. [Google Scholar]
- Sharma N, Charles C, Lynch M. Adjunctive benefit of an essential oil-containing mouthrinse in reducing plaque and gingivitis in patients who brush and floss regularly: a six-month study. J Am Dent Assoc. 2004;135(4):496-504. [Google Scholar]
- Löe H, Schiott R. The effect of mouthrinses and topical application of chlorhexidine on the development of dental plaque and gingivitis in man. J Periodontal Res. 1970;5(2):79-83. [Google Scholar]
- Tartaglia G, Tadakamadla S, Connelly S, Sforza C, Martín C. Adverse events associated with home use of mouthrinses: a systematic review. Ther Adv Drug Saf. 2019;10. [Google Scholar]
- Lata S, Varghese N, Varughese J. Remineralization potential of fluoride and amorphous calcium phosphate-casein phosphopeptide on enamel lesions: An in vitro comparative evaluation. J Conserv Dent. 2010;13(1):42-6. [Google Scholar]
- Pilli L, Singaraju G, Nettam V, Keerthipati T, Mandava P, Marya A. An extensive comparison of the clinical efficiency of acidulated phosphate fluoride (APF) and neutral sodium fluoride (NaF) oral rinses in the prevention of white spot lesions during fixed orthodontic treatment: a randomized controlled trial. Biomed Res Int. 2022;20(2):45-61. [Google Scholar]
- Jose J, Padmanabhan S, Chitharanjan A. Systemic consumption of probiotic curd and use of probiotic toothpaste to reduce Streptococcus mutans in plaque around orthodontic brackets. Am J Orthod Dentofac Orthop. 2013144;144(1):67-72. [Google Scholar]
- Shah SS, Nambiar S, Kamath D, Suman E, Unnikrishnan B, Desai A. Comparative evaluation of plaque inhibitory and antimicrobial efficacy of probiotic and chlorhexidine oral rinses in orthodontic patients. Int J Dent. 2019;18(6):18-22. [Google Scholar]
- Egbewale B. Random allocation in controlled clinical trials: a review. J Pharm Sci. 2014;17(2):248-53. [Google Scholar]
- Silness J, Löe H. Periodontal disease in pregnancy: correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22(1):121-35. [Google Scholar]
- Beberhold K, Sachse-Kulp A, Schwestka-Polly R, Hornecker E, Ziebolz D. The Orthodontic Plaque Index: an oral hygiene index for patients with multibracket appliances. Orthod Art Pract Dentofac Enhanc. 2012;13(1). [Google Scholar]
- Gorelick L, Geiger A, Gwinnett A. Incidence of white spot lesion after bonding and banding. Am J Orthod. 1982;81(2):93-8. [Google Scholar]
- Bilbilova E, Stefanovska E, Kapusevska B, Muratovska I, Kovacevska I. Clinical Study on the Effect of Chlorhexidine Mouth Rinse in Improving Oral Health in Orthodontic Patients with Fixed Appliances. Sylwan. 2015;159(3):432-47. [Google Scholar]
- Raju R, Divya A, Rajendran G, John J, John J. Analogous assay between green tea mouthwash, Listerine mouthwash, and chlorhexidine mouthwash in plaque reduction, on orthodontic patients: a randomized cross-over study. Int J Commun Med Public Health. 2017;4(5):1429-35. [Google Scholar]
- Hamdan A, Maxfield B, Tüfekçi E, Shroff B, Lindauer S. Preventing and treating white-spot lesions associated with orthodontic treatment: a survey of general dentists and orthodontists. J Am Dent Assoc. 2012;143(7):777-83. [Google Scholar]
- Abrol N, Singla A, Mahajan V, Jaj H, VS. Reliability of organic mouthwash compared to chlorhexidine mouthwash on Streptococcus mutans in the early phase of orthodontic treatment. J Indian Orthod Soc. 2015;49(4):188-92. [Google Scholar]
- Malik S, Halloli C, Shetty S, Tubaki R. Antimicrobial effect of herbal versus chemical mouthwashes in patients undergoing orthodontic treatment. Indian J Sci Res. 2019;9(2):63-8. [Google Scholar]
- Kaaij NVD, Veen MVD, Kaaij MVD, Cate J. A prospective, randomized placebo-controlled clinical trial on the effects of a fluoride rinse on white spot lesion development and bleeding in orthodontic patients. Eur J Oral Sci. 2015;123(3):186-93. [Google Scholar]
- Hadj-Hamou R, Senok A, Athanasiou A, Kaklamanos E. Do probiotics promote oral health during orthodontic treatment with fixed appliances? A systematic review. BMC Oral Health. 2020;20(1):1-9. [Google Scholar]
- Seidel C, Gerlach R, Weider M, Wölfel T, Schwarz V, Ströbel A. Influence of probiotics on the periodontium, the oral microbiota and the immune response during orthodontic treatment in adolescent and adult patients (ProMB Trial): study protocol for a prospective, double-blind, controlled, randomized clinical trial. BMC Oral Health. 2022;22(1):148-54. [Google Scholar]
- Ujgare S, Moolya N, Rajhans N, Daule N, Lawande A, Bhosale R. Clinical Evaluation of the Effects of Probiotics on Salivary Nitric Oxide Levels in Chronic Gingivitis Subjects during Orthodontic Treatment: A Clinico-Biochemical Study. Sch J Dent Sci. 2023;10(8):186-95. [Google Scholar]
- Kaaij NVD, Veen MVD, Kaaij MVD, Cate J. A prospective, randomized placebo-controlled clinical trial on the effects of a fluoride rinse on white spot lesion development and bleeding in orthodontic patients. Eur J Oral Sci. 2015;123(3):186-93. [Google Scholar]
- Andrucioli M, Amato P, Kuchler �, Matsumoto M, Bergamo A, Silva RD. Effect of chlorhexidine mouthwashes on periodontal parameters and extrinsic tooth staining in orthodontic patients. Am J Orthod Dentofac Orthop. 2023;164(6):855-61. [Google Scholar]
- Brightman L, Terezhalmy G, Greenwell H, Jacobs M, Enlow D. The effects of a 0.12% chlorhexidine gluconate mouthrinse on orthodontic patients aged 11 through 17 with established gingivitis. Am J Orthod Dentofac Orthop. 1991;100(4):324-9. [Google Scholar]
How to Cite This Article
Vancouver
Deora SK, Ganugapanta VR, Sankar SG, Bharghav R, Niharika UL, Mandava P. Evaluation of probiotic, chlorhexidine, and fluoride mouthwashes in orthodontic preventive care- A unicentric three-arm parallel randomized controlled trial [Internet]. J Contemp Orthod. 2024 [cited 2025 Oct 14];8(4):526-535. Available from: https://doi.org/10.18231/j.jco.2024.079
APA
Deora, S. K., Ganugapanta, V. R., Sankar, S. G., Bharghav, R., Niharika, U. L., Mandava, P. (2024). Evaluation of probiotic, chlorhexidine, and fluoride mouthwashes in orthodontic preventive care- A unicentric three-arm parallel randomized controlled trial. J Contemp Orthod, 8(4), 526-535. https://doi.org/10.18231/j.jco.2024.079
MLA
Deora, Shyama Kunwar, Ganugapanta, Vivek Reddy, Sankar, Singaraju Gowri, Bharghav, Rayala, Niharika, Ubbarapu Lakhsmi, Mandava, Prasad. "Evaluation of probiotic, chlorhexidine, and fluoride mouthwashes in orthodontic preventive care- A unicentric three-arm parallel randomized controlled trial." J Contemp Orthod, vol. 8, no. 4, 2024, pp. 526-535. https://doi.org/10.18231/j.jco.2024.079
Chicago
Deora, S. K., Ganugapanta, V. R., Sankar, S. G., Bharghav, R., Niharika, U. L., Mandava, P.. "Evaluation of probiotic, chlorhexidine, and fluoride mouthwashes in orthodontic preventive care- A unicentric three-arm parallel randomized controlled trial." J Contemp Orthod 8, no. 4 (2024): 526-535. https://doi.org/10.18231/j.jco.2024.079
