- Visibility 341 Views
- Downloads 48 Downloads
- Permissions
- DOI 10.18231/j.jco.2025.013
-
CrossMark
- Citation
A Comparative evaluation of the Shear bond strength of brackets bonded to pre-treated demineralised enamel treated with two different remineralising agents – An In-vitro study
Abstract
Background: Remineralising agents are suggested on sound enamel and on demineralised enamel during fixed appliance therapy as they increase the risk of enamel demineralization; but their influence on bond strength is questionable. Toothmin has been recently introduced and showed promising results in preventing demineralization and promoting remineralization similar to CPP-ACP.Therefore, the rationale of doing this study is to evaluate Toothmin efficacy on shear bond strength (SBS) of pre-treated demineralized enamel.
Aims: To measure the SBS of brackets bonded to pretreated demineralised enamel treated with Toothmin and CPP-ACP.
Settings and Design: Teeth were divided into four groups prior to bonding. Group I with No enamel pre-treatment, Group II, demineralized enamel, Group III, CPP-ACP was applied on demineralized enamel whereas in Group IV, Tooth min was applied on demineralised enamel.
Methods and Materials: Intact enamel group, demineralised group and remineralised groups were evaluated for SBS and (Adhesive Remnant Index ) ARI scores.
Statistical analysis: Data were analyzed using IBM SPSS version 20 software and subjedted to one way analysis of variance with Tukey’s post hoc tests.
Results and Conclusions: Toothmin group had highest mean SBS (10.37±3.08) followed by CPP-ACP (9.6±2.43), control (8.67±2.31), and the demineralization (2.42±1.21) groups. Highest mean ARI scores were observed in Toothmin group (2.33±0.48) and the least in the demineralization group (0.4±0.507).Demineralization of enamel significantly reduces the SBS of orthodontic brackets. Remineralization of enamel with Toothmin or CPP-ACP after demineralisation improved bond strength. Highest mean ARI scores were observed in Toothmin group and lowest in demineralized group.
Introduction
Fixed orthodontic appliances create problems in self-cleansing resulting in increased plaque retention and biofilm accumulation.[1], [2], [3], [4], [5] Studies shows that fixed orthodontic appliances compromises patients compliance towards oral hygiene maintenance.[6] and increases the risk of enamel demineralization. [7], [8], [9], [10]
Gorelick et al.[9] and Boersma et al.[11] reported the occurrence of early enamel lesions in 11- 24% of patients before orthodontic therapy and non developmental early enamel lesions in 50% of patients undergoing fixed orthodontic treatment. Tufekci et al[12] reported steady progress in the formation of WSLs from early months of orthodontic treatment to later stages.
Topical application of CPP-ACP paste and fluoride varnish, laser with fluoride,[13] laser with CPP-ACP, [14] laser with CPP-ACPF, [15] low-viscosity light-curing resin infiltration into deeper layers are the factors that can effect enamel lesions during fixed appliance therapy. [16]
Due to the increased occurence of enamel lesions during fixed appliance therapy, remineralising agents are suggested on sound enamel and on demineralised enamel but their influence on bond strength is questionable.
Several in vitro studies evaluated SBS after treatment of enamel surface with different preventive measures. [17] Previous literature revealed variable results like significant increase[18], [19] or decrease [20] or no variation in the SBS after pretreatment. [21], [22]
Toothmin has been recently introduced and showed promising results in its efficiency in preventing demineralization and promoting remineralization during orthodontic therapy similar to CPP-ACP.[23] CPP-ACP reduces demineralisation and promotes remineralisation by maintaining higher concentrations of calcium and phosphate mineral ion content on tooth surface. Toothmin toothpaste arrests the caries activity by maintaining higher concentrations of soluble calcium and phosphate ions which aids in better adsorption to the enamel surface.
Although it was proven that Toothmin is as effective as CPP-ACP in remineralising surface enamel. [23] however clinical data suggesting its effect on SBS of brackets attached to conditioned demineralised enamel surface is lacking. Therefore, the rationale of doing this in – vitro study is to evaluate the results of Toothmin and CPP-ACP paste application on SBS of pre-treated demineralized enamel.
From the previous research, the effect size was calculated to be 0.57 which is used to find out the sample size using G Power software. Sample size estimated to be 56 (rounded to 60) at a confidence interval of 95% and power of the study 95%. Based on 1:1 ratio 15 teeth per group was selected.
Teeth with good crown structure were included and teeth with decalcified enamel and which have undergone pre-treatment with surface reagents were excluded from the study.
Extracted premolars were stored in 0.1% thymol solution. Soft tissue remnants and callus was removed with a scaler. Each tooth was affixed vertically in a self-cure acrylic block so that the crown is exposed. Teeth were divided into four groups of 15 teeth each, as described in the following sections ([Figure 1]).
|
Group I |
No enamel pre-treatment (Control) |
|
Group II |
Demineralisation of enamel |
|
Group III |
CPP-ACP paste applied to demineralised enamel |
|
Group IV |
Toothmin applied to demineralised enamel |
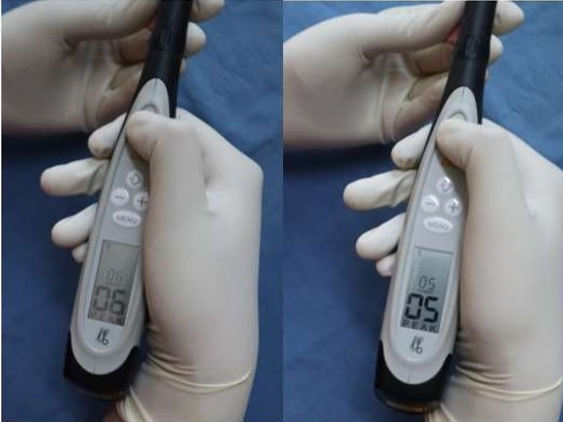
To establish a baseline, equal amount of mineral content of individual tooth was confirmed by a portable battery-powered laser fluorescence device DIAGNOdent Pen. Diagnodent readings were recorded for the groups I, II, III and IV to determine mineral content.
Demineralisation Process
The demineralization procedure was followed according to Wei Hua and John D. B. Featherstone10. With this procedure sequential demineralization and remineralization were performed in order to mimic the remineralizing stage of the caries process. Each premolar was kept in demineralization solution with acidic pH of 4.3 for 6 hours at 370C later washed with deionized water, and again kept in remineralization solution with neutral pH of 7.0 for about 18 hours. This was repeated daily for 3 weeks and on 21st day, teeth were dried and evaluated for frosty white appearance of enamel.
After demineralization, teeth were segregated into group III and IV. Mineral content was confirmed with the DIAGNOdent Pen and then stored in artificial saliva for around 30 days.
Group I: No enamel pre-treatment was done in this group.
Group II: In this group, bonding done on demineralized enamel.
Group III: In this group, application of CPP-ACP paste on demineralized enamel ([Figure 2]) was done prior to bonding. A cyclic application of CPP-ACP paste for 5 minutes followed by deionized water rinse for every 6 hours. Same procedure repeated for remineralisation process. A total of 10 cycles was done. During these cycles, teeth were stored in artificial saliva. Once demineralisation and remineralisation were done alternatively, brackets were bonded on the tooth surface.
Group IV: In this group, same protocol was followed as above instead, Tooth min ([Figure 2]) was used for CPP-ACP.
After remineralization of groups III and IV, Diagnodent readings ([Figure 3]) were taken to match the scores in both the groups.
Bracket bonding
Sixty stainless steel pre-adjusted edgewise maxillary bicuspid brackets with 0.022-inch slots (3M UNITEK) were adopted in this study. The buccal surfaces were cleansed for 5 seconds, washed for 10 seconds, and finally dried for about 10 seconds using an air-water syringe. Tooth surface etched with 37% Ortho-phosphoric acid followed by water rinse and then oil-free air applied for 10 sec till the surface appears frosty white. After conditioning with Primer, stainless-steel brackets were bonded to premolars with Trans bond XT and cured with LED. The specimens were kept in deionized water in a sealed container at room temperature for one day before debonding.
Debonding procedure and Shear bond strength testing
Brackets were subjected to debonding on Instron Testing Machine ([Figure 4]) and SBS was calculated for all the specimens. SBS obtained in Newtons from Insytron machine was converted to MPA by dividing the Force in Newton by Area of the bracket base (mm2).
Adhesive Remnant Index
A digital microscope with ×50 magnification was used to determine the mode of failure and the extent of remaining composite on the enamel ([Figure 5]). ARI scores at the failure area were recorded similar to the study by Artun and Bergland. [24]
The Adhesive Remnant Index
Index score Enamel Adhesive Remnant
No adhesive left on the enamel
Less than 50% of adhesive left on the enamel
More than 50% of adhesive left on the enamel
All adhesives left on the enamel
Statistical analysis
Data were analyzed using IBM SPSS version 20 software (IBM SPSS, IBM Corp., Armonk, NY, USA). Descriptive statistics, one way analysis of variance with Tukey’s post hoc tests, chi square test, Mann Whitney U tests, and Friedman’s tests were done to analyze the study data.
Results
resents the descriptive statistics for shear bond strength in the study groups. It was found that Toothmin group had highest mean shear bond strength (10.37±3.08) followed by CPP-ACP (9.6±2.43), control (8.67±2.31), and the demineralization (2.42±1.21) groups. These differences between groups were statistically significant ([Table 3]). In multiple pairwise comparisons, it was observed that the demineralization group had significantly lower shear bond strength compared to all other groups. While there was no statistically significant difference between CPP-ACP and Toothmin groups, both the groups demonstrated significantly higher shear bond strength compared to the control group ([Table 4]).
hows the comparison of ARI scores between the study groups. While ARI score 0 was most common in the demineralization group, score 2 was most common in the remaining three groups, the difference of which was statistically significant. [Table 6] presents the descriptive statistics for mean ARI scores in the study groups. Highest mean ARI scores were observed in Toothmin group (2.33±0.48) and the least mean score in the demineralization group (0.4±0.507). These differences between mean ARI scores were statistically significant ([Table 7]). In post hoc analysis, demineralization group demonstrated significantly lesser mean ARI scores compared to all the other three groups. No other pairwise comparisons were statistically significant.




|
Group |
N |
Mean |
Std. Deviation |
Std. Error |
95% Confidence Interval for Mean |
Minimum |
Maximum |
|
|
Lower Bound |
Upper Bound |
|||||||
|
Control |
15 |
8.6760 |
2.31508 |
.59775 |
7.7940 |
10.3580 |
6.41 |
13.95 |
|
Demineralization |
15 |
2.4293 |
1.21092 |
.31266 |
1.7587 |
3.0999 |
1.47 |
4.83 |
|
CPP-ACP |
15 |
9.6080 |
2.43913 |
.62978 |
7.7573 |
10.4587 |
6.13 |
13.95 |
|
Toothmin |
15 |
10.3793 |
3.08628 |
.79688 |
8.6702 |
12.0885 |
7.18 |
17.68 |
|
Group |
N |
Mean |
Std. Deviation |
Std. Error |
95% Confidence Interval for Mean |
F value |
P value |
|
|
Lower Bound |
Upper Bound |
|||||||
|
Control |
15 |
8.6760 |
2.31508 |
.59775 |
7.7940 |
10.3580 |
34.82 |
<0.001* |
|
Demineralization |
15 |
2.4293 |
1.21092 |
.31266 |
1.7587 |
3.0999 |
||
|
CPP-ACP |
15 |
9.6080 |
2.43913 |
.62978 |
7.7573 |
10.4587 |
||
|
Toothmin |
15 |
10.3793 |
3.08628 |
.79688 |
8.6702 |
12.0885 |
|
Reference Group |
Comparison Group |
Mean Difference |
P value |
95% Confidence Interval |
|
|
Lower Bound |
Upper Bound |
||||
|
Control |
Demineralization |
6.24667* |
.000 |
4.3637 |
8.9296 |
|
CPP-ACP |
-.93200 |
.041* |
-2.3149 |
-0.216 |
|
|
Toothmin |
-1.70333 |
.029* |
-3.5863 |
-0.9796 |
|
|
Demineralization |
CPP-ACP |
-7.17867* |
.000 |
-8.9616 |
-4.3957 |
|
Toothmin |
-7.95000* |
.000 |
-10.2329 |
-5.6671 |
|
|
CPP-ACP |
Toothmin |
-0.67133 |
.459 |
-3.5543 |
1.0116 |
|
Group |
ARI Score |
P value |
|||
|
0 |
1 |
2 |
3 |
||
|
Control |
0 |
2 (13.3) |
7 (46.7) |
6 (40) |
<0.001* |
|
Demineralization |
9 (60) |
6 (40) |
0 |
0 |
|
|
CPP-ACP |
0 |
0 |
11 (73.3) |
4 (26.7) |
|
|
Toothmin |
0 |
0 |
10 (66.7) |
5 (33.3) |
|
Group |
N |
Mean |
Std. Deviation |
Std. Error |
95% Confidence Interval for Mean |
Minimum |
Maximum |
|
|
Lower Bound |
Upper Bound |
|||||||
|
Control |
15 |
2.27 |
.704 |
.182 |
1.88 |
2.66 |
1 |
3 |
|
Demineralization |
15 |
.40 |
.507 |
.131 |
.12 |
.68 |
0 |
1 |
|
CPP-ACP |
15 |
2.27 |
.458 |
.118 |
2.01 |
2.52 |
2 |
3 |
|
Toothmin |
15 |
2.33 |
.488 |
.126 |
2.06 |
2.60 |
2 |
3 |
|
Group |
N |
Mean |
Std. Deviation |
Std. Error |
95% Confidence Interval for Mean |
F value |
P value |
|
|
Lower Bound |
Upper Bound |
|||||||
|
Control |
15 |
2.27 |
.704 |
.182 |
1.88 |
2.66 |
44.64 |
<0.001* |
|
Demineralization |
15 |
.40 |
.507 |
.131 |
.12 |
.68 |
||
|
CPP-ACP |
15 |
2.27 |
.458 |
.118 |
2.01 |
2.52 |
||
|
Toothmin |
15 |
2.33 |
.488 |
.126 |
2.06 |
2.60 |
Discussion
Development of White Spot Lesions (WSLs) is most commonly seen before and during fixed orthodontic treatment and their prevention is extremely important. Several authors reported prevalence of WSLs before orthodontic therapy to the extent of 11 to 24%. [9], [11] Use of pre-treatment agents in remineralizing these lesions would be beneficial because of high prevalence of WSLs (30-70%) during fixed orthodontic treatment; [25], [26], [27] but the effect of these agents on SBS of brackets is debatable.
Ideally, the bonded brackets should have bond strength ample enough to withstand the orthodontic and masticatory forces throughout the treatment duration but should be debonded at the end of the treatment with no damage to the tooth. [28]
In this study SBS of orthodontic brackets were tested on Intact enamel, after demineralization and after applying two different remineralising agents, CPP-ACP and Tooth Min. It was observed that Toothmin group had highest mean shear bond strength followed by CPP-ACP, Control, and the demineralization groups. There was no statistically significant difference between CPP-ACP and Toothmin groups, but demonstrated significantly higher shear bond strength in comparison with the control group.
To establish a baseline, equal amount of mineral content of each tooth was confirmed by laser fluorescence device DIAGNOdent Pen. Diagnodent readings were noted for the group I (Intact enamel), group II (Demineralised enamel), group III (CPP-ACP) and group IV (Toothmin) to determine mineral content. There was significant increase in the diagnodent scores following demineralization which reduced significantly after the application of remineralizing agent in both the CPP-ACP and the Toothmin groups which indicates the identical remineralisation capacity of both CPP-ACP and Toothmin.
Several methods for artificial demineralization of teeth are available to imitate primary caries lesions. For this purpose, Farhadian et al. [29] used the microbiological method, Baka et al. [30] and Veli et al. [31] used immersion in a demineralizing solution, and Uysal et al. [32] and Ekizer et al. [33] utilized a pH cycle. Marquezan et al. [34]
compared three tooth demineralization methods, which includes the use of an acid gel, a pH cycle, and microbiological method and concluded that the use of a pH cycle was more effective than an acid gel. Hence in the current study, pH cycle advocated by Hu and Featherstone [10] was adopted. 21 days of pH cycling [32] resulted in good frosty enamel surface in contrast to 14 days cycle. [10] Artificial caries lesions are quite similar but not identical to natural caries lesions which aids in the possibilty of testing invitro. [35]
Extracted teeth are routinely stored in aqueous solutions till the required number were collected in Invitro studies.[36] Habelitz et al [37] study observed, a 25% reduction in the hardness of tooth when they were stored in distilled water for one day. According to Aydin et al. [36] study, 0.1% Thymol solution as storage medium is best in maintaining the mineral content of the enamel. Therefore, they were stored in Thymol solution till all the teeth were collected in the current study. In between the cycles of demineralisation and remineralisation, teeth were kept in artificial saliva to simulate the oral environment.
Current study observed least SBS in demineralized specimens compared to other groups which can be accredited to the poor quality of the surface enamel and the lack of resin tags that form the mechanical interlock. Application of adhesive resin after enamel demineralization led to evenly distributed rows of tags.[38] Highest SBS was observed in Toothmin group followed by CPP-ACP followed by Intact Enamel group and demineralised group the least SBS with statistically significant difference. Highest mean bond strength observed in Toothmin group compared to CPP-ACP could be the result of the availability of greater mineralized ions in a soluble form at high concentrations in Toothmin providing the increased mineralized content thereby increased SBS. Incipient enamel lesions occur by loss of minerals beneath the surface layer. [39] Since enamel minerals are effective in establishing a good bond, [40] this factor decreases SBS of brackets to demineralized enamel. Current study results were acceptable as SBS values of all the groups were higher than the Reynold [41] suggested values (5.9– 7.8 MPa) except in demineralisation group.
In Keles and P. Daneshkazemi [42] studies higher SBS of brackets were found in intact enamel groups than demineralized enamel groups with significant difference between them.In Uysal [32] study, SBSs of CPP-ACP treated samples were higher compared to the demineralization group, and there were no significant differences between the control and CPP-ACP treated groups. It would be reasonable to think that CPP-ACP led to an identical enamel surface composition as observed in the control group.
Similar to the present study findings, Kecik et al.[43] and Xianojun et al. [44] found that the SBS of CPP-ACP treated samples were higher than that of the control group.Quite contrast to the other studies, in Gulec and Goymen [45] study no statistically significant difference was observed in SBS of intact enamel compared to demineralized enamel. These differences in SBS in various studies could be due to usage of different bonding materials, prolonged use of remineralising agents and storage time of teeth in artificial saliva.
To overcome the short comings of other studies[45] differences in tooth demineralisation protocols and no standardization of demineralization quantification,DIAGNOdent device was used in the present study to measure the quantity of mineral content in all the groups.
The amount of remaining adhesive on the enamel surface after bracket debonding is routinely evaluated by Adhesive remnant index. [46] But the efficiency of the ARI to reflect the bond strength is questionable.[31], [47], [48], [49], [50], [51] The lesser the adhesive remnant on the enamel post debonding, the safer the enamel cleanup. [49], [52] However lesser the risk of enamel fracture during bracket removal with the presence of minimal composite remaining at the enamel surface. [50], [51], [52], [53]
In this study, highest mean ARI scores were observed in Toothmin group and the least mean score in the demineralization group with statistically significant difference. In contrast to the present study, Nabawy et al. [54] study showed no statistically significant differences regarding ARI scores between the 3 groups where most of the scores were either 1 or 2 in all the groups, which indicates a cohesive failure.[55] Cohesive failures offer the enamel surface protection by reducing the possible risk of enamel fracture during debonding as well as enamel damage during enamel clean-up post debonding.
Similar to the current study, Cossellu et al.[49] and Uysal et al [32] studies also reported that groups with greater bond strength often exhibit ARI score of 1 and 0 respectively. However Ekizerstudy[33] reported recurrent ARI scores of 2 and 3 in demineralized group and APF gel treated demineralized enamel group respectively.
Variations in demineralization procedures, rate of thermal cycling, the rod movement speed in Instron machine,storage environment, pre-treatment agents application methods and the bracket base used[42] would have affected results from different studies. In order to replicate the oral environment, extracted human premolars teeth were used in the current study rather than bovine teeth which were shown to have two or three times faster dissolving capacity than human enamel, [56] and teeth were stored in artificial saliva. [57], [58]
However, it is not possible to replicate the oral environment in in-vitro studies which is considered as the major limitation of the current study. Therefore it is preferable to conduct in-vivo studies to test the failure rate of orthodontic brackets bonded after CPP–ACP application and Toothmin.
Results concluded from the present study were as follows:
Demineralization of enamel significantly reduces the SBS of orthodontic brackets.
Remineralization of enamel with Toothmin or CPP-ACP after demineralisation improved bond strength.
Both Toothmin and CPP-ACP pretreatment are equally efficient as remineralising agents and for bonding orthodontic brackets.
Highest mean ARI scores were observed in Toothmin group with lesser failures at the composite-enamel interface and lower ARI scores with highest failures at composite-enamel interface were observed in untreated demineralized group.
Source of Funding
None.
Conflict of Interest
None.
References
- Arici S, Alkan A, Arici N. Comparison of different toothbrushing protocols in poor toothbrushing orthodontic patients. Eur J Orthod. 2007;29(5):488-92. [Google Scholar]
- Koopman J, Kaaij NVD, Buijs M. The effect of fixed orthodontic appliances and fluoride mouthwash on the oral microbiome of adolescents-A randomized controlled clinical trial. PLoS One. 2015;10(9). [Google Scholar]
- Ren Y, Jongsma M, Mei L, Mei HVD, Busscher H. Orthodontic treatment with fixed appliances and biofilm formation - A potential public health threat?. Clin Oral Invest. 2014;18(7):1711-9. [Google Scholar]
- Gomes S, Varela C, Veiga SD, Rösing C, Oppermann R. Periodontal conditions in subjects following orthodontic therapy. A preliminary study. Eur J Orthod. 2007;29(5):477-81. [Google Scholar]
- Ristic M, Vlahovicsvabic M, Sasic M, Zelic O. Clinical and microbiological effects of fixed orthodontic appliances on periodontal tissues in adolescents. Orthod Craniofac Res. 2007;10(4):187-95. [Google Scholar]
- Suri AT, Suri S, Tompson B. Predictors of adolescent compliance with oral hygiene instructions during two-arch multibracket fixed orthodontic treatment. Angle Orthod. 2011;81(3):525-56. [Google Scholar]
- Zachrisson B, Zachrisson S. Caries incidence and oral hygiene during orthodontic treatment. Eur J Oral Sci. 1971;79(4):394-401. [Google Scholar]
- Mizrahi E. Enamel demineralization following orthodontic treatment. Am J Orthod. 1982;82(1):62-7. [Google Scholar]
- Gorelick L, Geiger A, Gwinnett A. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982;81(2):93-8. [Google Scholar]
- Hu W, Featherstone J. Prevention of enamel demineralization: an in-vitro study using light-cured filled sealant. Am J Orthod Dentofac Orthop. 2005;128(5):592-600. [Google Scholar]
- Boersma J, Veen MVD, Lagerweij M, Bokhout B. Prahl-Andersen B. Caries prevalence measured with QLF after treatment with fixed orthodontic appliances: influencing factors. Caries Res. 2005;39(1):41-8. [Google Scholar]
- Tufekci E, Dixon J, Gunsolley J, Lindauer S. Prevalence of white spot lesions during orthodontic treatment with fixed appliances. Angle Orthod. 2011;81(2):206-16. [Google Scholar]
- Allam G, Aziz A. Comparing topical fluoride application, laser irradiation and their combined effect on remineralisation of enamel. Futur Dent J. 2018;4(2):318-41. [Google Scholar]
- Yassaei S, Aghili H, Shahraki N, Safari I. Efficacy of erbium-doped yttrium aluminum garnet laser with casein phosphopeptide amorphous calcium phosphate with and without fluoride for remineralization of white spot lesions around orthodontic brackets. Eur J Dent. 2018;12(2):210-6. [Google Scholar]
- Nair A, Kumar R, Philip S, Ahameed S, Punnathara S, Peter J. A comparative analysis of caries inhibitory effect of remineralizing agents on human enamel treated with Er: YAG laser: an in-vitro atomic emission spectrometry analysis. J Clin Diagn Res JCDR. 2016;10(12):10-3. [Google Scholar]
- Tinanoff N, Baez R, Guillory D, C. Early childhood caries epidemiology, aetiology, risk assessment, societal burden, management, education, and policy: Global perspective. Int J Paediatr Dent. 2019;29(3):238-86. [Google Scholar]
- Yomna A, Tarek N, Yousry N. El Harouni Shear bond strength of metallic brackets bonded to enamel pretreated with Er, Cr: YSGG LASER and CPP-ACP. BMC Oral Health. 2021;21(1). [Google Scholar]
- Khargekar N, Kalathingal J, Sam G, Elpatal M. Evaluation of diferent pretreatment efcacy with fluoride-releasing material on shear bond strength of orthodontic bracket: an in vitro study. J Contemp Dent Pract. 2019;20(12):1442-6. [Google Scholar]
- Al-Kawari H, Am A. Effect of diferent preventive agents on bracket shear bond strength: in vitro study. BMC Oral Health. 2014;14. [Google Scholar]
- Çehreli S, Şar �, Polat-Özsoy �, Ünver B, Özsoy S. Effects of a fluoride containing casein phosphopeptide-amorphous calcium phosphate com plex on the shear bond strength of orthodontic brackets. Eur J Orthod. 2012;34(2):193-200. [Google Scholar]
- Bağlar S, Sub-Ablative E. Cr: YSGG laser irradiation under all-ceramic resto rations: effects on demineralization and shear bond strength. Lasers Med Sci. 2018;33(1):41-50. [Google Scholar]
- Jesus TD, Bezerra G, Souza PD, Torres C. Yag pre-treatment for bonding of orthodontic bracket: 1 year of in vitro treatment. Clin Cosmet Investig Dent. 2017;9:19-25. [Google Scholar]
- Prasad N, Kumar T, Sharma T. Gauravchaudhary and Rithikagupta. Assessment for the efficacy of various remineralising agents during fixed orthodontic mechanotherapy: in vivo study. Int J Curr Res. 2018;10(4):67731-70. [Google Scholar]
- Artun J, Bergland S. Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am J Orthod. 1984;85(4):333-40. [Google Scholar]
- Topaloglu-Ak A, Ertugrul F, Eden E, Ates M, Bulut H. Effect of orthodontic appliances on oral microbiota-6-month follow-up. J ClinPediatr Dent. 2011;35(4):433-9. [Google Scholar]
- Enaia M, Bock N, Ruf S. White-spot lesions during MB appliance treatment: a challenge for clinical excellence. Am J Orthod Dentofac Orthop. 2011;140(1):17-24. [Google Scholar]
- Richter A, Arruda A, Peters M, Sohn W. Incidence of caries lesions among patients treated with comprehensive orthodontics. Am J Orthod Dentofac Orthop. 2011;139(5):657-64. [Google Scholar]
- Bakhadher W, Halawany H, Talic N, Abraham N, Jacob V. Factors affecting the shear bond strength of orthodontic brackets-a review of in vitro studies. Acta Medica (Hradec Kral Czech Republic). 2015;58(2):43-51. [Google Scholar]
- Farhadian N, Rezaei-Soufi L, Jamalian F. Effect of CPP-ACP paste with and without CO2 laser irradiation on demineralized enamel microhardness and bracket shear bond strength. Dental Press J Orthod. 2017;22:53-60. [Google Scholar]
- Baka Z, Akin M, Ileri Z, Basciftci F. Effects of remineralization procedures on shear bond strengths of brackets bonded to demineralized enamel surfaces with self-etch systems. Angle Orthod. 2016;86:661-8. [Google Scholar]
- Veli I, Akin M, Baka Z, Uysal T. Effects of different pretreatment methods on the shear bond strength of orthodontic brackets to demineralized enamel. Acta Odontol Scand. 2016;74(1):7-13. [Google Scholar]
- Tancanuysal A, Banuuysalc M, Aydınbelged T, Al-Qunaian. Do fluoride and casein phosphopeptide-amorphous calcium phosphate affect shear bond strength of orthodontic brackets bonded to a demineralized enamel surface?. Angle Orthod. 2011;81(3):490-5. [Google Scholar]
- Ekizer A, Zorba O, Uysal Y, Ayrikcil T. Effects of demineralization-inhibition procedures on the bond strength of brackets bonded to demineralized enamel surface. Korean J Orthod. 2012;42(1):17-22. [Google Scholar]
- Marquezan M, Corrêa F, Sanabe M. Artificial methods of dentine caries induction: A hardness and morphological comparative study. Arch Oral Biol. 2009;54(12):1111-8. [Google Scholar]
- Arends J, Christoffersen J. Invited review article: the nature of early caries lesions in enamel. J Dent Res. 1986;65(1):2-11. [Google Scholar]
- Aydın B, Pamir T, Baltaci A, Orman M, Turk T. Effect of storage solutions on microhardness of crown enamel and dentine. Eur J Dent. 2015;9(2):262-8. [Google Scholar]
- Habelitz S, Marshall G, Balooch m, Marshall S. Nanoindentation and storage of teeth. J Biomech. 2002;35(7):995-8. [Google Scholar]
- Zachrisson B, Graber T, BS. Bonding in orthodontics. Orthodontics: Current Principles and Techniques. 1985. [Google Scholar]
- Murphy T, Willmot D, Rodd H. Management of post orthodontic demineralized white spot lesions with microabrasion: a quantitative assessment. Am J Orthod Dentofac Orthop. 2007;131(1):27-33. [Google Scholar]
- Nisha G, Amit G. . Textbook of Operative Dentistry. 2010. [Google Scholar]
- Reynolds I. A review of direct orthodontic bonding. Br J Orthod. 1975;2(3):171-9. [Google Scholar]
- Pedramdaneshkazemi S, Khodaei M. Shear bond strength of orthodontic brackets on intact and demineralized enamel after application of resin infiltrant, fluoride varnish and casein phosphopeptideamorphous calcium phosphate remineralizing agents: in-vitro study. Int Orthod. 2021;19(2):259-68. [Google Scholar]
- Kecik D, Cehreli S, Sar C, Unver B. Effect of acidulated phosphate fluoride and casein phosphopeptide-amorphous calcium phosphate application on shear bond strengths of orthodontic brackets. Angle Orthod. 2008;78(1):129-33. [Google Scholar]
- Xiaojun D, Xuehua G, Jing L, Hong R, Youcheng Y, Zhangyu G. Effects of CPP-ACP paste on the shear bond strength of orthodontic brackets. Angle Orthod. 2009;79(5):945-50. [Google Scholar]
- Gulec A, Goymen M. Assessment of the resin infiltration and CPP-ACP applications before orthodontic brackets bonding. Dent Mater J. 2019;38(5):854-60. [Google Scholar]
- Montasser M, Drummond J. Reliability of the adhesive remnant index score system with diferent magnifications. Angle Orthod. 2009;79(4):773-9. [Google Scholar]
- Naseh R, Fallahzadeh F, Atai M, Mortezai O, Setayeshrad R. Casein phosphopeptideamorphous calcium phosphate effects on brackets shear bond strength and enamel damage. J Clin Exp Dent. 2017;9(8):1002-9. [Google Scholar]
- Cacciafesta V, Sfondrini MF, Calvi D, Scribante A. Effect of fluoride application on shear bond strength of brackets bonded with a resin-modified glass-ionomer. Am J Orthod Dentofac Orthop. 2005;127(5):580-3. [Google Scholar]
- Cossellu G, Lanteri V, Butera A, Sarcina M, Farronato G. Effects of six different preventive treatments on the shear bond strength of orthodontic brackets: in vitro study. Acta Biomater Odontol Scand. 2015;1(1):13-20. [Google Scholar]
- Henkin FD, Macêdo �D, Santos KD, Schwarzbach M, Samuel S, Mundstock K. Effects of six different preventive treatments on the shear bond strength of orthodontic brackets: in vitro study. Dent Press J Orthod. 2016;21(6):67-73. [Google Scholar]
- Dilip S, Noufal S, Ravi M, Krishnaraj K, Charles R. Comparison of surface roughness of enamel and shear bond strength, between conventional acid etching and erbium, chromium-doped: Yttrium scandium gallium garnet laser etching-an in vitro study. Dent Res J (Isfahan). 2018;15(4):248-55. [Google Scholar]
- Cehreli S, Polat-Ozsoy O, Sar C, Cubukcu H, Cehreli Z. A comparative study of qualitative and quantitative methods for the assess ment of adhesive remnant after bracket debonding. Eur J Orthod. 2012;34(2):188-92. [Google Scholar]
- Mirhashemi A, Sharif N, Kharazifard M, Jadidi H, Chiniforush N. Com parison of the adhesive remnant index and shear bond strength of orthodontic brackets using acid etch versus Er: YAG laser treatments. Laser Phys. 2019;29(11). [Google Scholar]
- Nabawy Y, Tarek N, Yousry NE. Shear bond strength of metallic brackets bonded to enamel pretreated with Er, Cr: YSGG LASER and CPP-ACP. BMC Oral Health. 2021;21(1). [Google Scholar]
- Pires-De-Souza F, Filho B, Sousa A, Chinelatti M. Shear bond strength of orthodontic brackets after accelerated artifcial aging. J Dent. 2013;56(1):35-41. [Google Scholar]
- Featherstone J, Melberg J. Relative rates of progress of artifcial carious lesions in bovine, ovine and human enamel. Caries Res. 1981;15(1):109-23. [Google Scholar]
- Gale M, Darvell B. Thermal cycling procedure for laboratory testing of dental restorations. J Dent. 1999;27(2):89-99. [Google Scholar]
- Dijken J, Ruyter I. Surface characteristics of posterior composites after polishing and toothbrushing. Acta Odontol Scand. 1987;45(5):337-83. [Google Scholar]
How to Cite This Article
Vancouver
Shaik SN, Mallavarapu K, Revathi P, Lanka D, Dokku A, Pichai S. A Comparative evaluation of the Shear bond strength of brackets bonded to pre-treated demineralised enamel treated with two different remineralising agents – An In-vitro study [Internet]. J Contemp Orthod. 2025 [cited 2025 Nov 02];9(1):97-104. Available from: https://doi.org/10.18231/j.jco.2025.013
APA
Shaik, S. N., Mallavarapu, K., Revathi, P., Lanka, D., Dokku, A., Pichai, S. (2025). A Comparative evaluation of the Shear bond strength of brackets bonded to pre-treated demineralised enamel treated with two different remineralising agents – An In-vitro study. J Contemp Orthod, 9(1), 97-104. https://doi.org/10.18231/j.jco.2025.013
MLA
Shaik, Shafeen Naqheeb, Mallavarapu, Kalyani, Revathi, P., Lanka, Devikanth, Dokku, Aruna, Pichai, Saravanan. "A Comparative evaluation of the Shear bond strength of brackets bonded to pre-treated demineralised enamel treated with two different remineralising agents – An In-vitro study." J Contemp Orthod, vol. 9, no. 1, 2025, pp. 97-104. https://doi.org/10.18231/j.jco.2025.013
Chicago
Shaik, S. N., Mallavarapu, K., Revathi, P., Lanka, D., Dokku, A., Pichai, S.. "A Comparative evaluation of the Shear bond strength of brackets bonded to pre-treated demineralised enamel treated with two different remineralising agents – An In-vitro study." J Contemp Orthod 9, no. 1 (2025): 97-104. https://doi.org/10.18231/j.jco.2025.013
